Pain relief in Labour
Datin Dr (Mrs) Kamaljit Kaur Manocha, M.D. (UKM) M.Med. O & G (UKM)
Consultant Obstetrician & Gynaecologist
Bangsar Women Specialist Centre, Kuala Lumpur, Malaysia
What is labour pain?
Labour begins when your uterus starts to contract. A few days before labour starts, you may experience a tightening of the uterus which could cause discomfort rather than pain.
Labour is said to start when you get regular contractions. Contractions increase in frequency and intensity throughout labour, and can become painful in a way that is similar as the pain you may experience in other muscles of your body when you do vigorous exercise.
At the same time, the opening into the uterus – the cervix – is stretching to eventually allow your baby to pass through your birth canal.
When the opening to the cervix is fully dilated, you begin what is known as the second stage of labour, which is when your baby is born. The baby passes through your birth canal and is born through a combination of the continuing contractions of your uterus and a conscious effort to push your baby out by using the muscles of your lower abdomen.
How does my body cope with the pain?
During your pregnancy, changes happen in your body to prepare for these events. The ligaments of your pelvis loosen to permit your pelvis to relax and allow your baby to come out. Other changes occur to adapt your body to accommodate childbirth. Unfortunately, despite these changes, it is likely you will feel pain. First labours are probably more painful than subsequent ones.
Sometimes, when it is necessary to induce labour or stimulate it if progress is slow, your labour may be more painful.
Every person”s tolerance of pain is different, and what one person can accept, another may find extremely painful.
What contributes to more pain?
Pain can be worsened by
· A big baby
· Baby with a malposition
· Poor maternal health (fatigue, high blood pressure)
· Poor breathing techniques (slow, deeper breathing is the best way to release muscle tension)
· Poor preparation of labour or anxiety (counter-productive to physical pain)
· Poor positioning of mother
How does one cope better with labour pain?
Be prepared
Preparing for childbirth during your pregnancy can improve these natural changes. At childbirth classes, you will be advised on exercises to make you fitter, besides relaxation and breathing exercises to help you manage your labour pains. Sometimes this is all that you may need.
Take good care of yourself
Watching your diet, and not smoking are other ways you can help yourself besides improving your fitness and training your body for the task that lies ahead. Massaging certain areas of the body will help compete with the pain message to the brain, reducing the sensation of pain.
Supportive partner
Having a birthing partner who is calm, supportive and loving is very comforting because you are not alone. A friendly atmosphere with homely surroundings and good and encouraging medical staff are assets in reducing pain in labour.
Experienced midwife
A midwife will spend most of the time with you during labour. Midwives are trained and licensed to administer pain relief. They are able to seek assistance to administer other methods of pain relief. Midwives are also involved in giving advice at antenatal classes.
Pain relief
Gentle exercise, breathing, posture and relaxation techniques help in early labour. A warm bath may also help. Transcutaneous Electrical Nerve Stimulation (TENS) may be of help in early labour. Physiotherapists may also be involved and can give advice on TENS.
What are the analgesics available in the Labour Suite?
Breathing/Inhalational Pain Relief (Entonox)
Entonox is available in most labour suites and consists of 50% oxygen and 50% nitrous oxide. It is inhaled through a mask when a contraction is coming on, to provide temporary pain relief in the late first stage or second stage of labour. It is safe for both mother and baby as the gases do not accumulate in the body.
Injectable analgesia (Pethidine)
Pethidine is a common pain relief given in most labour suites as an injection on the buttock. It is also a sedative and helps the labouring mum to relax/sleep.
However, in almost half of these women, it causes nausea or vomiting and, hence, has to be given with an anti-vomiting injection. It also induces drowsiness in the mother, and, if given too close to the time of birth, might cause drowsiness in the baby as it crosses the placental barrier.
Sometimes the baby might have to be given an injection (Narcaine) to counteract the effect of the medication.
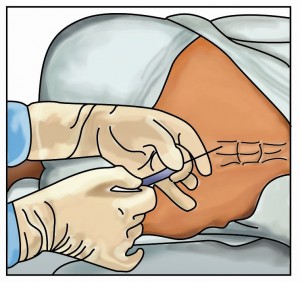
Epidural block
Epidurals are a form of ”regional anaesthesia”. This means they are aimed at preventing pain sensations (and to a certain degree, touch and temperature sensations) from being felt in a ”region” of the body.
An epidural affects the lower region of the body. The medication injected into the epidural space during labour is intended to prevent the woman from feeling pain. An epidural is often referred to as an ”epidural block” (EDB), as it works by ”blocking” pain sensations.
EDB requires the involvement of a skilled and experienced anaesthetist for its institution and management. The pain relief provided by the epidural block is far superior to any other pain relief in labour. The process of labour is monitored continuously by qualified staff.
Side effects are minimal; apart from the numbness of the lower half of the body, there is a possibility of reduced desire by the labouring mother to bear down during the second stage of labour – which might need encouragement. Therefore, the anaesthetist usually reduces the concentration of the drug in the second stage so that some sensation is felt, enabling her to push successfully. Mild shivering is possible and usually short lived.
Obstetricians are doctors specialising in the medicine of childbirth. They may have knowledge in administering some forms of pain relief including some local anaesthetic techniques involved in childbirth.
Anaesthetists are specialist doctors with knowledge and experience in providing all types of pain relief and can apply more sophisticated forms of pain relief to you in labour, in addition to anaesthetics, if necessary.
TENS
TENS has been used for pain relief in labour and is said to be effective particularly in early labour.Treatment with TENS consists of attaching pads to your back. A low voltage electric current is passed through these pads and this stimulates your body to produce its own natural pain relieving substances. It takes about 30 minutes before an effect is felt. The pain relief achieved is usually assessed as moderate, and is sometimes inconsistent. There are no known ill effects from TENS. or some women, it is of considerable value. As labour progresses, the intensity of the electrical stimulation can be increased to cope with the increased pain of contractions, but, frequently, stronger pain relief may be required.
It is important for couples to attend antenatal classes to be able to obtain further information and make an informed consent on their method of pain relief, if any is required at all.
RECOMMENDED BOOKS:
[easyazon-image align=”none” asin=”B008LW1KBW” locale=”us” height=”160″ src=”http://ecx.images-amazon.com/images/I/517n98O8GsL._SL160_.jpg” width=”120″] [easyazon-image align=”none” asin=”B000AM24E8″ locale=”us” height=”146″ src=”http://ecx.images-amazon.com/images/I/51F83BWATKL._SL160_.jpg” width=”160″] [easyazon-image align=”none” asin=”1558326723″ locale=”us” height=”160″ src=”http://ecx.images-amazon.com/images/I/517R5HrLqLL._SL160_.jpg” width=”107″] [easyazon-image align=”none” asin=”1558320431″ locale=”us” height=”160″ src=”http://ecx.images-amazon.com/images/I/51EGm6IwthL._SL160_.jpg” width=”105″]